HHS Budget Cuts and Their Potential Effects on Hospitals
Potential Implications for Healthcare Access and Financial Stability
Overview of HHS Budget Cuts
The recently proposed fiscal year 2025 budget reductions to the Department of Health and Human Services (HHS) present a serious concern for hospitals and the communities they serve. With an overall $7.5 billion (6.4%) decrease compared to 2024, the budget includes:
- Medicaid Reductions: Up to $880 billion in cuts over eight years, jeopardizing access to care.
- Program Eliminations: Termination of funding for Title X Family Planning, the Ending the HIV Epidemic initiative, and maternal/child health programs like Healthy Start.
- Public Health Cuts: Closure of half of HHS regional offices, elimination of preventive health block grants, and reduced infectious disease surveillance funding.
- Workforce Reductions: 20,000 HHS personnel, including researchers, clinicians, and administrative support, face layoffs.
Rising Healthcare Insecurity
These proposed cuts come at a time when more Americans than ever are already struggling to access affordable care. According to the 2024 Gallup and West Health Healthcare Indices Study, 11% of U.S. adults are now considered “cost desperate,” meaning they were recently unable to afford needed care or medication, the highest level recorded since the survey began in 2021.
The study highlights worsening disparities: 25% of households earning under $24,000, 18% of Hispanic adults, and 14% of Black adults reported being desperate. Meanwhile, 64% of households earning under $48,000 and 57% between $24,000 and $48,000 said they struggle to access affordable care, significantly up from the previous year. In contrast, no meaningful change was seen among white adults or higher-income groups, underscoring a growing divide.
The share of Americans who are “cost secure,” those who can afford care and medication, has fallen to just 51%, a record low. Gallup and West Health warn that this “erosion of cost security in healthcare” signals that the affordability gap between the haves and have-nots is more expansive than ever.
Impacts on Hospitals: RCA’s Observations
As a trusted partner to hospitals for over 30 years, Resource Corporation of America (RCA) understands these cuts’ profound and immediate impact on hospital operations, particularly those supporting underserved populations.
- Financial Instability for Safety-Net Hospitals
Hospitals that depend on Medicaid reimbursements, especially safety-net and rural facilities, will face increased financial strain. Medicaid currently accounts for roughly 19% of hospital revenue; its reduction may force hospitals to scale back services or, in the worst cases, shut down critical care units or entire facilities.
In addition, the defunding of long-term care centers and local clinics will further stress hospital emergency rooms as patients lose access to proactive and preventive services.
- Erosion of Access to Care
The Gallup data affirms that Americans are already struggling to access affordable healthcare. Cuts to Medicaid and preventive programs will only deepen the crisis, leaving hospitals to absorb the burden of increased emergency visits, delayed diagnoses, and worsening health outcomes. - Public Health Infrastructure Breakdown
Hospitals will be less equipped to coordinate care and respond to health crises without support from HHS public health programs. The loss of surveillance infrastructure and community health worker initiatives will significantly impact hospitals’ ability to manage chronic diseases and respond to outbreaks effectively. - Workforce Disruption and Reduced Coordination
The layoff of thousands of public health professionals diminishes the collaborative network hospitals rely on for outreach, education, and emergency preparedness. As federal staffing support dwindles, hospitals must find new ways to bridge gaps in care coordination and public health response.
Long-Term Risks to Healthcare Sustainability
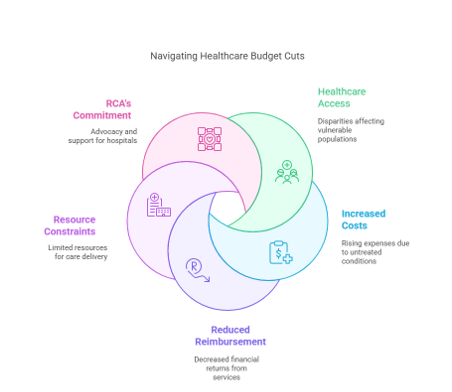
The downstream effects of these budget cuts are likely to deepen inequities in healthcare access, particularly for low-income populations. As untreated conditions escalate and healthcare utilization patterns shift, hospitals will face increased costs, reduced reimbursement, and mounting pressure to deliver care with fewer resources.
RCA’s Commitment
At RCA, we recognize the importance of preserving access to care for vulnerable populations. These budget changes and the findings from Gallup highlight the urgent need for innovative, data-driven solutions to help hospitals recover lost revenue, navigate complex funding environments, and connect patients with available federal, state, and hospital-sponsored financial assistance programs.
More than ever, hospitals need experienced partners to strengthen eligibility services, accelerate conversions, and ensure no patient falls through the cracks.
Conclusion
The proposed HHS budget cuts and the growing population of cost-desperate Americans present a dual threat to the nation’s health system. RCA stands with hospitals in calling for reevaluating these reductions and remains committed to helping healthcare organizations safeguard access and stabilize their financial future.

Leave A Comment
You must be logged in to post a comment.