You’ve probably felt the financial squeeze lately if you work in hospital administration or revenue cycle management. Between looming cuts to the 340B Drug Pricing Program and reductions in Medicaid Disproportionate Share Hospital (DSH) payments, it’s getting harder to make the numbers work, primarily if your hospital serves many uninsured or underinsured patients.
But here’s the thing: while we can’t control every change coming down from Washington or the pharmaceutical industry, there’s one area where hospitals have real power: making sure every eligible patient is identified and qualified for the right programs to preserve the associated Medicaid days.
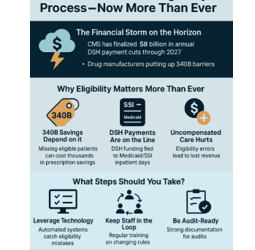
The Financial Storm on the Horizon
Let’s get specific. CMS has finalized $8 billion in annual DSH payment cuts through 2027. Unless your hospital is in the top percentile for serving low-income patients, you will likely see your share of those dollars shrink. And 340B? Drug manufacturers are putting up more barriers, especially around specialty drugs. Some hospitals are losing millions every year because they can’t access the same discounts they once did.
This isn’t just a budget headache. Real money pays for real care, everything from cancer treatments to emergency surgeries for patients with nowhere else to turn.
Why Eligibility Matters More Than Ever
So, what can you do? The answer is simple but powerful: get your patient eligibility process in the best shape possible.
Here’s why it matters:
- 340B Savings Depend on It: If you miss a patient who qualifies for 340B, you could lose thousands of dollars on a single prescription. Those losses add up fast.
- DSH Payments Are on the Line: DSH funding is tied to how many Medicaid and SSI inpatient days you can document. If your numbers are off, your payments could take a hit—right when you need them most.
- Uncompensated Care Hurts: Every eligibility error is a missed opportunity to get reimbursed. Even a small percentage of errors can cost your hospital hundreds if not millions, each year.
What Steps Should You Take?
Here’s what we’re seeing work for hospitals that want to stay ahead:
- Leverage Technology: Automated systems that check insurance and Medicaid status in real-time can catch mistakes before they become costly.
- Keep Staff in the Loop: Regular training is essential. The rules are changing, and your team needs to stay sharp.
- Be Audit-Ready: Good documentation isn’t just about compliance—it’s your best defense if you’re ever audited or challenged on your numbers.
The Real Cost of Doing Nothing
Let’s be honest: hospitals are already running lean. If you lose $1 million in 340B savings, you’d need to generate $5–$7 million in new revenue to make up for it. That’s a tall order in today’s environment.
If DSH payments drop, it’s not just a line item; it’s fewer resources for patient care, staff, and community programs.
The Bottom Line
There’s a lot we can’t control in healthcare right now. But is it essential to ensure every eligible patient is counted and qualified? That’s squarely in our hands.
Investing in your eligibility process isn’t just about compliance. It’s about protecting your hospital’s mission and ensuring you can keep serving those who need you most.
If you haven’t reviewed your process lately, now’s the time.
Contact RCA today to discover how our proven eligibility solutions can help you offset 340B and DSH reductions, reduce uncompensated Care, and maximize your reimbursements.
Let’s build a stronger, more resilient revenue cycle—together.
Get started with RCA now.

Leave A Comment
You must be logged in to post a comment.